Phantom Limb
Phantom limbs
occur in 95 to 100 percent of amputees who lose an arm or leg. The phantom is
usually described as having a tingling feeling and a definite shape that
resembles the somatosensory experience of the physical limb before amputation.
It is reported to move through space in much the same way as the normal limb
would move when the person walks, sits down, or stretches out on a bed. At
first, the phantom limb feels perfectly normal in size and shape -- so much so
that the amputee may reach out for objects with the phantom hand, or try to
step onto the floor with the phantom leg. As time passes, however, the phantom
limb begins to change shape. The arm or leg becomes less distinct and may fade
away altogether, so that the phantom hand or foot seems to be hanging in
midair. Sometimes, the limb is slowly "telescoped" into the stump
until only the hand or foot remains at the stump tip.
Phantom Limbs
Christy Taylor
Phantom Limb Pain (PLP) is a serious condition that occurs when a person who has lost a part of their body though amputation, trauma (brachial plexus), or loss of nervous connections in an appendage, perceives that the limb is still there and experiences sensations coming from this area. It was first described in 1866 by S. Weir Mitchell, an American neurologist, through a short story published in Atlantic Monthly. While Mitchell may then have wondered if this was specific to wounded Civil War soldiers, it has since been established as quite common (1). Over 70% of amputees report phantom limb pain for years after amputation (2). Several theories have been proposed regarding PLP, although there is still much to be learned and understood. Early physicians believed that phantom limb sensations were caused by severed nerves that fired randomly, sending signals to the somatosensory cortex re-creating sensations seemingly coming from the missing limb. However, this theory was soon disproved when surgeons tried unsuccessfully to eradicate these sensations by cutting the nerves leading to the neuromas, preventing the neuromal signals from reaching the cortex. Researchers then began to concentrate on the role of the spinal cord in PLP, but realized that paraplegics with completely severed spinal cords still experienced sensations where their limbs had been (5). Focus then turned to the brain and its role.
Until the mid 1980's, it was widely believed that once neural pathways were placed during fetal development, these pathways did not change and were not altered in any recognizable way (3). However, recent studies have shown that the brain has a high degree of plasticity into adulthood, which allows it to continually respond to changes in stimuli (4). A study done by Flor, et al., in 1995 showed a relationship between the amount of cortical reorganization and the magnitude of phantom limb pain. Data indicated that PLP is related to, and may be a consequence of, plastic changes in the primary somatosensory cortex, and that the shift of the cortical map following amputation might be a potential neurophysiological basis of PLP (6).
Further studies in 1998 investigating the re-mapping component in the brain were conducted by researchers at the University of Toronto and The Toronto Hospital. The study recruited amputees who experienced phantom pain for surgery to map the sensory areas in the brain. During the mapping process, the conscious patients reported sensations they felt when certain areas of the thalamus were stimulated. Patients reported phantom sensations when areas of the thalamus were stimulated that formally were innervated by neurons from the missing arm, and also when areas on the stump were stimulated that activated these reorganized regions in the brain. Neurons were shown to continue to carry out their original roles, but with different sources of activation (7).
Other researchers, such as Vilayanur Ramachandran had other answers to the question of phantom pain aetiology. He was inspired by previous experiments by Michael Merzenich that had studied the homunculus (blueprint representation of the entire body surface, which identifies the locations of sensations felt on the skin) of monkeys. In these experiments, the sensory nerves in the arms of a group of monkeys were severed. It was found that that despite the lack of sensory input from the arm, the arm region of the body map in the cortex hadn't gone silent. Instead, signals from the face (next door on the map) had taken over for the phantom arm (9). They concluded that there were existing axon branches that become unmasked when normal input had disappeared (11) .
Ramachandran wondered if amputees who complained of phantom pain could be suffering from rearranged body maps, and formulated his cortical remapping theory. He examined the reorganized homunculus of patients with removed limbs. By using q-tips to brush the face of a patient, he was able to produce sensations in their phantom limb. So each time a patient smiled or scratched their face, they stimulated the arm region of the body map causing a sensation in their phantom limb (9). Paralysis occurred because even after the limb was severed, the brain continued to send signals commanding the missing limb to move. This created an illusion of movement as the brain still monitored the intention. As a result of the absence of visual and proprioceptive activation, the different signals feeding into the body image contradicted each other. Ultimately the brain learned to interpret the lack of response as paralysis of the non-existent limb (9).
Ramachandran reasoned that in order to treat the paralysis, it was necessary to eliminate the discrepancy by allowing the patient to see the movement they wanted to make. He developed an ingenious method using mirrors that provided the brain with this visual stimulation. A midvertical sagittal mirror was put in front of the patient, and they placed their remaining limb in an exact mirror-symmetric location opposite to their phantom limb (12). The reflection the intact limb was optically superimposed on the perceived location of the phantom limb (12). Ramachandran has been successful with helping patients ease the pain for their phantom limbs using this therapy. Six of ten patients instantly felt their paralyzed phantom limbs moving, and a few were able to shift their phantom limbs out of painfully awkward positions (12). One patient even managed to correct his body image, and his phantom limb eventually shrank away to nothing (12).
While persuasive, the aforementioned experimental conclusions are well critiqued by Ronald Melzack who argues against looking to the somatosensory cortex or thalamus as the only cause of phantom pain in his April 1992 Scientific American article. He states: Such changes in the somatosensory thalamus or cortex could explain why certain feelings arise in limbs that no longer exist or can no longer transmit signals to the brain. Nevertheless, alterations in this system cannot by themselves account for phantoms and their pain. If this explanation were sufficient, removal of the affected parts of the somatosensory cortex or thalamus would solve both problems (1).
Melzack goes on to suggest that much more of the cerebrum, or the cerebral hemispheres, is involved with PLP, and introduces the concept of "neurosignature" or "neuromatrix (1). Melzack defines a neurosignature as a "network of neurons, that, in addition to responding to sensory stimulation, continuously generates a characteristic pattern of impulses indicating that the body is intact and unequivocally one's own" (1). Melzack states that the "matrix of wholeness" established in the brain will continue to operate even in the absence of sensory inputs, and would create an impression of having a complete and whole body even when a limb has been removed (1).
Pain-related phenomena may be due, in part, to inconsistencies between the corollary discharge signals sent to the brain for processing and those sent by the sensory system. Corollary discharge signals are used to define expectation, and when the sensory input does not match this expectation, the nervous system sends out a signal that says "there is something wrong" which may be felt as pain in the phantom limb. Melzack also describes the pain phenomena through his neuromatrix. He states that the neuromatrix is prewired to "assume" that the limbs can move, and that when they do not, stronger and more frequent messages may be sent to the muscles, and is perceived as pain (1). Interesting findings regarding treatment of phantom limb pain also indicate that more than the somatosensory cortex is involved with the pain felt by phantom limb sufferers. In the past, the success rate for treatment of phantom pain has been negligible, with only about one percent of treated amputees reporting any relief lasting for a year. However, recently, the use of electromyographic and temperature feedback has proven effective for patients with cramping and burning phantom pain. The aim of the treatment is to teach amputees to unconsciously keep their phantom limb as warm as their intact limb (8). This treatment may somehow allow the corollary discharge and sensory system signals to agree with one another or may allow the patient to resist fighting his or her prewired neuromatrix. It also suggests further study of the integration of perception and reality with regard to phantom limb pain management. Another unconventional pain management technique is continuous electrical stimulation through electrodes surgically implanted into the thalamus. This technique blocks neuronal activity in the thalamus that may be the cause of some phantom pain (10).
References
1. Melzack, Ronald, Scientific American. "Phantom Limbs"
2. Katz, Joel, "Phantom Limb Pain. (Commentary)"
3. Yang, Tony T., Gallen C., Schwartz, B., Bloom, F.E., Ramachandran, S. Cobb, "Sensory Maps in the Human Brain," Nature, vol. 368, 14 April 1994: 592-593.
4. "Cortical Reorganization and the 'Phantom Limb'"
5. "Plasticity"
6. Flor, H., Elbert,T., Knecht, S., Wienbruch, C., Pantev, C., Birbaumer, N., Larbig, W., Taub, E., "Phantom Limb Pain as a Perceptual Correlate of Cortical Reorganization Following Arm Amputation," Nature, vol. 375, 8 June 1995: 482-483.
7. "New Piece to Puzzle in Phantom Pain Mystery: Media Release from the University of Toronto"
8. Sherman, Richard, "The Use of Electromyographic and Temperature Biofeedback for Treatment of Cramping and Burning Phantom Limb Pain"
10. "Phantom Pain Not Imagined," The University of Toronto
9. THEY
DO IT WITH MIRRORS , From New Scientist
11. Phantom
Homepage, Macalester Psychology page
12. Ramachandran, V.S. & Rogers-Ramachandran, D. "Phantom Limbs and Neural Plasticity." in Archives of Neurology. Vol. 57 (pg. 317-320), 2000, Ramachandran article
Episodic Analgesia |
(I) The
condition has no relation to the severity or the location of the injury.
(2) There is no simple relationship to
circumstances — Some of the injuries occurred
during military combat, whereas others occurred in more mundane settings such
as work.
(3) The victim can be fully aware of the nature of the
injury but feel no pain.
(4) The analgesia is instantaneous.
(5) The analgesia lasts for a limited time.
(6) The analgesia is localised to the injury — the patient might experience no pain at the severed limb but
complain about the needle prick for an injection.
Phantom limb pain Melzack (1992) 7 features (See Banyard and Grayson 1st ed p384, 2nd
ed p387)
- Phantom limb feels real. Sometimes amputees try to walk on their phantom limb.
- Phantom arm hangs down at the side when resting. Appears to swing in time with other arm, when walking.
- Sometimes gets stuck in awkward position. If behind the patients back, then patient feels obliged to sleep on stomach.
- Artificial limb appears to fit like a glove. See artificial limb as part of their body.
- Phantom limbs give impression of pressure and pain
- Even if phantom limb is experienced as spatially detached from the body, it is still felt to belong to the patient.
- Paraplegic people experience phantom limbs. They can even experience continually cycling legs.
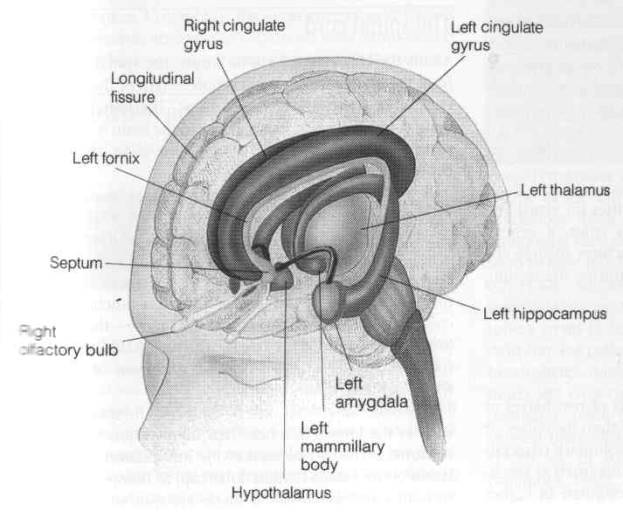
Melzack’s Model
The matrix has at least three major nerve circuits:
- Sensory pathways passing through the thalamus and sensory cortex
- Emotional and motivational pathways passing through the limbic system
- Pathways associated with the recognition of self, which is commonly thought to involve the parietal lobe of the cortex. Studies of people with damage to the parietal lobe have shown problems with their sense of self, for example some patients have been known to push one of their own legs out of bed because they are were convinced that it belongs to a stranger.
The phenomenon of phantom limbs highlights the problems with simple reductionist explanations of behaviour and experience (the attempt to explain our complex feelings and behaviour in terms of simple biological responses).